|
Lehigh BioE now offers an undergraduate degree in biocomputational engineering! Check out the video above for more. |
Welcome to Lehigh's Department of Bioengineering!
At Lehigh, we believe that the greatest potential for innovation occurs at the boundaries between strong disciplines. At the core of Lehigh’s Department of Bioengineering are pillars of recognized strengths in bioscience, systems, mechanics, materials and computer science, and our Department upholds a strong tradition of interdisciplinary thinking as our faculty and students work closely with peers from around the world to develop breakthrough innovations and technologies focused on alleviating problems related to human health.
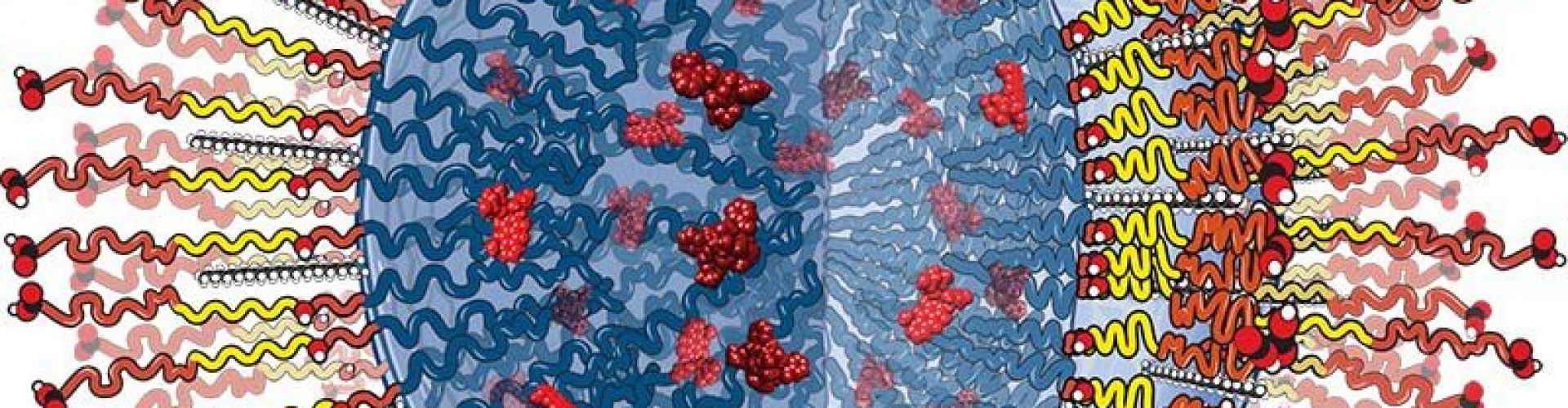
Our research areas span key areas such as biocomputation and modeling, diagnostics, sensors and devices, and materials and therapies, and the outcomes of our faculty-led efforts are contributing to advances in tissue engineering and regenerative medicine, the development of platforms for the early detection of disease and precision diagnostics, and the design of novel biological pharmaceuticals and nanomedicine, biosensors and medical devices. | MORE >>
Department News
Spring 2024 BioE Seminar: Li Shen
Celebrate the 2024 Undergraduate Research Symposium winners!

Read the Lehigh Bioengineering 2023-24 Newsletter:
- Machine learning & brain biomarkers may hold the key to precision mental health diagnosis and care
- Engineering Technologies for Health
- Making it Together to Make A Difference
- Extending the Reach of Healthcare Through Technology
- Building Global Connections: Lehigh BioE Establishes Partnerships and Extends its Impact
- BioE Graduate Research:
- A 3D Tumor Model to Improve Preclinical Drug Discovery
- Unraveling the Mechanisms of Olfaction Through Molecular Modeling
- A More Robust In Vitro Model To Assess Smooth Muscle Cell Behavior
- 2023 Spotlight: Faculty awards, Recent Publications, Media Mentions, Graduate Student News, Alumni Updates, and Student Success